CARDIAC INVESTIGATIONS
COMMON CARDIAC TESTS
Why do I need a 24-hour blood pressure monitor test?
Blood pressure varies through the day due many factors (exercise, rest, sleep, medication etc) and so a one-off reading is not the best way to diagnose high blood pressure.
A 24 hour monitor captures measurements throughout the day and night allowing us to get a clear idea of your ‘normal’ blood pressure.
We will not use a single measurement to diagnose ‘high blood pressure’.
How is the monitor fitted?
It is a good idea to wear a loose-fitting top or shirt to your appointment as this makes it easier to fit the monitor. We will fit the inflatable cuff on the arm of your choice. It should sit comfortably around your arm so please reposition it if needed. If the cuff moves during the monitoring period, the results may not be accurate. The cuff is connected to a small monitor, which you will wear around your waist clipped into a belt or waistband. It takes about 10 minutes to fit the cuff and monitor.
Results
You will be asked to return the monitor to us, normally the following day. There is a short turnaround time while we analyse the results. We will send these results through to you with advice on the next step.
Patch tests are new and small devices that are unobtrusive, simple to apply, and easy to remove. They allow heart rhythms to be monitored for up to two weeks. It is applied just under the left collarbone, or over the breastbone, by gently pressing the adhesive layer to your skin. They can be worn in the shower, and allow all normal physical activities to take place. After the monitoring period is completed, we ask that you simply peel the device away from your skin, and return it in the provided prepaid box which you post in a normal mailbox. This is then received by an analysis centre in the UK which allows cardiac analysts to create a detailed report. This is then analysed and interpreted by your cardiologist.
What happens during a Holter monitor test?
The Holter monitor is the size of a mobile phone and attaches to your chest via three leads. The monitor can sit in your pocket hang around your neck. You will be asked to keep a diary of any symptoms you experience during the recording period. The recording is designed to sample you normal active daily living so you will be encouraged to go about your normal routine.
What happens after?
The Holter monitor records all of your heart beats in every 24 hours, over 115,000 if your average rate is 80 bpm. It takes a little while to go through this data to establish if the rhythm is normal. A report will be produced and your cardiologist will explain the findings to you.
What happens during an ETT?
The exercise test (or “stress test”) is conducted in a closely supervised situation. You will be attached to the ECG recording monitor just as you were for the resting ECG. You will then stand on a treadmill, which will begin to move very slowly. Progressively, as you become accustomed to the pace, the workload will be increased. All the time, we will be monitoring your heart rate, blood pressure and looking carefully at the ECG for any changes. You will be asked to report any chest pain/tightness during the test. You may stop the test at any point.
What happens following the test?
You will be allowed to recover whilst we monitor the ECG and when your heart rate and blood pressure have returned to normal, the test is completed. The cardiologist will review and analyse your exercise test .
When do we need a cardiac MRI?
A cardiac MRI is one of the best ways to take detailed pictures of the heart and how it moves in major different conditions of the heart including:
- Heart failure (where the heart is not pumping as well) and to assess what the cause might be
- Congenital heart disease (heart problems that developed in the womb)
- Some heart muscle conditions, such as cardiomyopathy
- Heart valve disease
- Assess the blood supply to the heart muscle
What happens during a cardiac MRI?
- You will be asked to lie on a bed, which moves inside a tunnel-shaped scanner. The scanner is open at both ends.
- You’ll be asked to lie still while the scan is taking place.
- The scan may last for up to an hour, but there’s a buzzer you can press if you need to speak to the radiographer (the person operating the scanner).
- The scanner is quite noisy. You’ll be able to hear banging sounds but you’ll usually be offered earplugs or earphones so you can listen to music.
- For some cardiac MRIs the doctor will use a dye known as contrast agent so that the images of blood flow to your heart show up more clearly on the scan. The dye will be injected into a vein in your arm. Your doctor will give you more information about this if it’s required.
Credit: British Heart Foundation – Your guide to a cardiac MRI, heart disease test
Can everyone have a cardiac MRI?
Most people can have an MRI scan, but there are certain patients that cannot. Before the MRI an extensive questionnaire will be undertaken to assess you before you have the scan.
You need to tell the MRI team if you have a pacemaker or implantable defibrillator. Most modern devices are safe in an MRI scanner, but it will need to be checked as it can affect some device and the settings.
You cannot have an MRI if you have inner ear implants or any type of surgical foreign body such as a metal clip in the brain or eye.
All patients will need a recent blood test to check kidneys prior to an MRI.
Where do we perform cardiac MRI’s?
We refer patients to our local partner centres in Bristol, Oxford or Birmingham.
What happens after
Once the images are taken they are reported and sent to the cardiologist, who will inform you of the results and any recommendations.
What is a CTCA?
A CTCA is a special type of scan that lets us look at your heart arteries (coronary arteries). CTCA is a very common test to investigate chest pain amongst other symptoms. A CTCA lets us take very detailed pictures of the heart and coronary arteries.
How is a CTCA carried out?
A CTCA is performed on a CT scanner by a specialised team. A radiographer when you are ready will take you into the scanning room and lie you on a specialised bed built into the scanner. They will place some sticky pads called electrodes on to your chest so the activity of your heart can be monitored during the scan. Your heart rate is monitored to allow us to take high quality pictures. The scanner consists of a large ring containing an X-ray tube (looks similar to a large polo mint) which your bed will move through, the scan itself is painless.
The team will place a small needle (cannula) in a vein to allow us to give specialised dye at the time of the scan to see the blood vessels clearly.
Your heart rate has to be well controlled for the test. If it is elevated then some medication (beta blockers) may need to be given to help control the heart rate. It only has a short-term effect and is very safe. It allows the pictures to be clearer.
A radiographer / nurse will go through a checklist before the test to check all your details. It is important you let us know all the relevant information and if you have any allergies.
Where are these tests performed?
We perform this test at either Gloucester Royal Hospital or Cheltenham General Hospital
Results
The results will be sent to your doctor who will interpret the results with your clinical information, determining a recommended management plan.
If a coronary angiogram is recommended, Dr McAloon will refer you to one of his expert colleagues who specialise in this field.
Credit: British Heart Foundation – Your guide to a Coronary Angiogram, a test for heart disease
Sensors attached to the skin are used to detect the electrical signals produced by your heart each time it beats. These signals are recorded by a machine for the healthcare professional to look at.
An ECG is often used alongside other tests to help diagnose and monitor conditions affecting the heart. It can be used to investigate symptoms of a possible heart problem, such as chest pain, palpitations (suddenly noticeable heartbeats), dizziness and shortness of breath.
It is a very important investigation if you are having your heart assessed.
ECHOCARDIOGRAMS
You may have already had an Echocardiogram (sometimes just called ‘echo’) performed. This is a non-invasive imaging test using ultrasound to look at your heart. Ultrasound is a very high-frequency sound which cannot be heard by the human ear. It is used to gain information regarding the structure and function of the heart muscles, chambers of the heart and structures within the heart such as the valves. The test is painless and does not use radioactivity.
A Bubble Contrast Echocardiogram uses imaging ultrasound combined with an injection of micro bubble contrast to help determine additional information.
Why am I being asked to come in for this test?
Your doctor suspects that you may have a hole in your heart. The majority of significant holes in you heart are detected in childhood. However, if there is a small defect or hole in the wall (inter-atrial septum) separating the left and right upper chambers of the heart (atria), this may not come to light until adulthood. The microbubble contrast allows for the detection of these small holes as they do not usually show up on a normal Transthoracic Echocardiogram.
Why might there be a defect in this part of my heart?
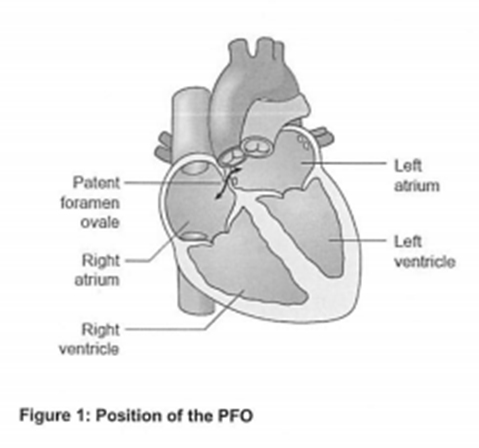
During the normal development of the foetal heart, there is an opening through the inter-atrial septum which allows blood to bypass the lungs which are not being used. Normally, this opening closes in the first few days or weeks after birth, but if it does not, the child will have a communication between the left and right atria.
This may take the form of a hole (Atrial Septal Defect – ASD) or a small channel (Patent Foramen Ovale – PFO) which behaves rather like a “trapdoor”. The defect will often correct itself without any medical intervention before the child reaches the age of 2, but about 25 to 30% of adults in the general population are said to have a PFO.
What happens if I have a PFO?
Many people do not have any symptoms or problems because of this defect, and it is detected by chance. However, some people have symptoms of breathlessness or fatigue (tiredness) due to some of the blood circulation bypassing the lungs (known as a shunt).
In other people, symptoms can result from blood clots forming in one of the veins in the leg (a deep vein thrombosis – DVT) and then a fragment of clot (embolus) passes from the right to the left side of the heart; this may block an artery resulting in:
• Stroke (loss of brain function).
• Heart attack (damage to the heart muscle)
What is a Bubble Contrast Echocardiogram?
You may have already had an Echocardiogram (sometimes just called ‘echo’) performed. This is a non-invasive imaging test using ultrasound to look at your heart. Ultrasound is a very high-frequency sound which cannot be heard by the human ear. It is used to gain information regarding the structure and function of the heart muscles, chambers of the heart and structures within the heart such as the valves. The test is painless and does not use radioactivity.
A Bubble Contrast Echocardiogram uses imaging ultrasound combined with an injection of micro bubble contrast to help determine additional information.
Why am I being asked to come in for this test?
Your doctor suspects that you may have a hole in your heart. The majority of significant holes in you heart are detected in childhood. However, if there is a small defect or hole in the wall (inter-atrial septum) separating the left and right upper chambers of the heart (atria), this may not come to light until adulthood. The microbubble contrast allows for the detection of these small holes as they do not usually show up on a normal Transthoracic Echocardiogram.
Why might there be a defect in this part of my heart?
During the normal development of the foetal heart, there is an opening through the inter-atrial septum which allows blood to bypass the lungs which are not being used. Normally, this opening closes in the first few days or weeks after birth, but if it does not, the child will have a communication between the left and right atria.
This may take the form of a hole (Atrial Septal Defect – ASD) or a small channel (Patent Foramen Ovale – PFO) which behaves rather like a “trapdoor”. The defect will often correct itself without any medical intervention before the child reaches the age of 2, but about 25 to 30% of adults in the general population are said to have a PFO.
What happens if I have a PFO?
Many people do not have any symptoms or problems because of this defect, and it is detected by chance. However, some people have symptoms of breathlessness or fatigue (tiredness) due to some of the blood circulation bypassing the lungs (known as a shunt).
In other people, symptoms can result from blood clots forming in one of the veins in the leg (a deep vein thrombosis – DVT) and then a fragment of clot (embolus) passes from the right to the left side of the heart; this may block an artery resulting in:
• Stroke (loss of brain function).
• Heart attack (damage to the heart muscle)
Alternative reasons to perform this test may include:
• Extra communications (small holes) between blood vessels in your lungs (known as pulmonary arterio-venous malformations).
• Chronic liver disease.
What does the Bubble Contrast Echocardiogram involve?
• You will be taken into a room with usually a doctor and a sonographer.
• You will be asked to undress to the waist and will be offered a hospital gown that should be left open at the front (like a coast). You will then be asked to lie on a bed. ECG stickers will be attacked to your chest and connected to the Echocardiogram machine. This will monitor your heart rate and rhythm throughout the test.
• You will have a small plastic tube (cannula) inserted into one of the veins in you arm. This will be used later for the injection of microbubbles. You will then be asked to lie onto your left side hand side. If you are unable to lie on your left side, we can carry out the test while you are lying on your back. This test is performed in semi-darkness so the lights will be dimmed once you are comfortable.
• The sonographer will place this Echocardiogram probe on your chest (this is like a thick blunt pen) and cold lubricating jelly (this helps get good contact with the skin).
• If you have already had a Transthoracic Echocardiogram, we will go straight on to perform the bubble contrast study. If not, a number of pictures of the heart will be recorded from different areas of your chest.
• Once the baseline study has been completed, we will go on to the bubble contrast study. The bubbles are made up in a syringe using sterile saline (salty water) mixed with a little bit of air and a little bit of your blood drawn back from the vein via the cannula.
• These are rapidly missed up to make very tiny microbubbles which are then injected into your vein. We will record pictures and watch carefully to see if any bubbles cross through from the right to the left side of the heart.
• You will then be asked to cough and sniff, and with further injections you will need to perform a special breathing and blowing technique called Valsalva manoeuvre; this will be carefully explained to you and practiced afterwards before we undertake this part of the test on the day.
• This test will take about 30 to 45 minutes to complete.
Do I need to take any special precautions before this test?
No, you should take all your usual medications as normal on the day of the test. You can also eat and drink normally. We advise that you keep hydrated (having plenty to drink) and keep yourself warm before the test. This increases the chance that we can access a vein for the cannula insertion during the test.
Is injecting air into the bloodstream harmful?
If a large amount of ait was injected into a vein as a large bubble, it could potentially cause harm, however the bubbles injected in this test are very small. If there is no hole in the inter-atrial septum, the bubbles will simply be filtered out by the lungs.
If you have Patent Foramen Ovale (PFO) some bubbles will appear on the left side of the heart and then will gradually make their way through the circulation and be filtered out through the lungs.
Risks, contra-indications and side effects:
• The Valsalva manoeuvre involves breathing techniques to change the pressures in your chest. This may lead to your ears ‘popping’ or a slight headache. If you have any ear problems, you should let the doctor know at the start of the test.
• Some people find performing the Valsalva manoeuvre difficult, but we can help you practice as much as we need to and can often still get reasonable images even if the technique cannot be perfected.
• The test does not carry any specific risks; ultrasound waves are harmless (they are used on pregnant women), no chemicals or contrast agents are used, so even if you have been allergic to X-ray contrast in the past that does not stop you from having this test.
• If you are on any blood thinning medication, you may bleed or bruise more easily when the cannula is removed.
After the procedure:
You may be given the results immediately, but some findings take longer to interpret and may need a second opinion. If there is a hole, the doctor will explain this. The results will be sent to your referring doctor.
Further information:
What is it?
An echocardiogram or ‘echo’ is a scan that uses ultrasound (sound waves) to produce pictures of the heart. The test is painless and does not use radioactivity. During a Contrast Echo a Contrast agent is injected which improves the quality of the images that are being recorded.
Why is it being done?
If your Doctor has decided that you need an Echocardiogram, but the picture quality is not very good, a contrast agent can be used to help improve the images. A Contrast Echo is also used to help diagnose if you have any holes in the heart.
What does it involve?
You will be taken into a darkened room. One or two people will usually be present. The person performing the test is called a Sonographer, who may be male or female. The Sonographer will usually NOT be a doctor. This means that some questions you may have about the result may have to wait until you see your doctor in clinic.
You will be asked to undress to the waist and put on a gown that should be left open to the front. You will be asked to lie on a couch on your left hand side.
Stickers will be attached to your chest and connected to the machine. These will be used to monitor your heart rate during the test. A drip will be placed in your arm.
The Sonographer will record a number of pictures of the heart. Whilst this is happening, a contrast agent will be injected into the drip to improve the quality of the images. If the Doctor is looking for the presence of a hole in the heart, you may be asked to cough and sniff whilst the images are being recorded.
The echocardiogram will take approximately 30-40 minutes to complete.
Are there any special precautions that I need to take before the echocardiogram?
No. You can take all your medication as normal. You can eat and drink as normal.
At the end of your echocardiogram
Once the echocardiogram is complete you can get dressed and leave. There are no limitations to what you can do after the scan, for example, you may drive.
Are there any risks in having the Contrast Echo?
There is an extremely small risk (less than 1 in 10,000) of developing an allergic reaction to the contrast agent used. If you have had allergic reactions to any medicines before please inform us before starting the test.
What is it?
An echocardiogram or ‘echo’ is a scan that uses ultrasound (sound waves) to produce pictures of the heart. The test is painless and does not use radioactivity. During an Exercise Echo, your Doctor will ask you to walk on a treadmill or ride an exercise bike whilst pictures are taken of your heart.
Why is it being done?
An Exercise Echo is performed as it allows your Doctor to understand how the heart copes when it is made to work harder. An Exercise Echo is useful to diagnose whether you have angina or not. It can also give your Doctor information about the severity of a heart-valve problem.
What does it involve?
You will be taken into a darkened room. Three people will usually be present when you have the test – a Doctor, a Sonographer and an assistant.
You will be asked to undress to the waist and put on a gown that should be left open to the front. You will be asked to lie on a couch on your left hand side.
Stickers will be attached to your chest and connected to the machine. These will be used to monitor your heart rate. Your blood pressure will also be checked regularly throughout the test. A drip may be placed in the vein in your arm, if the doctor needs to inject contrast which improves the quality of the images recorded.
Pictures of your heart will be recorded on the machine. You will then be asked to exercise, either by walking on a treadmill or riding an exercise bike. The exercise will be gentle at first but will get progressively more strenuous. Occasionally the Sonographer may record pictures of your heart whilst you are exercising.
When the Doctor has decided that you have performed enough exercise, or if you are unable to continue, the Doctor will ask you to lie back on the couch and more images of the heart will be recorded. You will continue to have your heart rate and blood pressure monitored until you have fully recovered, which may take several minutes.
Overall the Exercise Echo will take around 30-45 minutes to complete.
Are there any special precautions that I need to take before the exercise echo?
You must NOT take beta-blocker or calcium-channel blocker tablets for 48 hours before the test. Beta-blocker tablets include Atenolol, Bisoprolol and Carvedilol, although there are others. Calcium-channel blockers are called Diltiazem and Verapamil. These tablets prevent the heart from working hard. If you do continue with beta-blocker or calcium- channel blocker drugs, the Exercise Echo may need to be postponed. If you have any doubts, please contact your Doctors’ secretary or this unit.
You should continue other medications as usual.
At the end of your echocardiogram
You will be able to return home after the test has been completed. You may undertake your day-to-day activities as usual.
Are there any risks in having the exercise echo?
The Exercise Echo scan is extremely safe as it is just like exercising as if you were at home. There is an extremely small risk (less than 1 in 10,000) of developing an allergic reaction if contrast is used. If you have had allergic reactions to any medicines before please inform your Doctor before starting the test.
If you suffer with angina, there is an extremely small risk (less than 1 in 10,000) you may have a small heart attack during the test.
What is it?
An echocardiogram or ‘echo’ is a scan that uses ultrasound (sound waves) to produce pictures of the heart. The test is painless and does not use radioactivity. During a Pharmacological Stress Echo, your Doctor will give you some medicine to make the heart beat harder and faster whilst pictures are taken of your heart.
Why is it being done?
A Stress Echo is performed as it allows your Doctor to understand how the heart copes when it is made to work harder. A Stress Echo is useful to diagnose whether you have angina or not. It can also give your Doctor information about the severity of a valve problem, and it can help your Doctor to decide whether your heart function will improve after a by-pass operation.
What does it involve?
You will be taken into a darkened room. Two or three people will usually be present when you have the test – a Doctor, a Sonographer and occasionally an assistant.
You will be asked to undress to the waist and put on a gown that should be left open to the front. You will be asked to lie on a couch on your left hand side.
Stickers will be attached to your chest and connected to the machine. These will be used to monitor your heart rate. Your blood pressure will also be checked regularly throughout the test.
A drip will be put in the vein in your arm. Some ‘stress’ medicine will be infused into the drip, which makes the heart work harder. Whilst this is happening the Sonographer will take pictures of your heart using an ultrasound probe gently placed on your chest.
During the test the Doctor may also inject a contrast agent into the drip in your arm. This helps to improve the quality of the pictures that are being recorded.
When your heart has been made to work hard enough, the Doctor will stop the medicine. The Sonographer will continue to take pictures of the heart, and you will continue to be monitored until the effects of the stress medicine have worn off. This may take several minutes.
Overall the Stress Echo takes around 45 minutes to complete.
Are there any special precautions that I need to take before the stress echo?
You must NOT take beta-blocker or calcium-channel blocker tablets for 48 hours before the test. Beta-blocker tablets include Atenolol, Bisoprolol and Carvedilol, although there are others. Calcium-channel blockers are called Diltiazem and Verapamil. These tablets prevent the stress medicine from making the heart work harder. If you do continue with beta-blocker or calcium-channel blocker drugs, the Stress Echo may need to be postponed. If you have any doubts, please contact your Doctors’ secretary or this unit.
You should continue other medications as usual.
You must NOT eat for two hours before the test, but you may drink water.
At the end of your stress echo
After the echo you will occasionally be asked just to sit quietly for around 20 minutes to make sure the effects of the stress medicine have completely worn off.
You will be able to return home after this. It is advisable that you do not drive yourself for the remainder of the day, so you may need a friend or relative to transport you.
Will I be aware of anything during the stress echo?
The stress medicine will make your heart beat harder and faster, which you may notice. Occasionally the stress medicine may make you feel sick or dizzy. Let your Doctor know of any symptoms you are aware of. Once the stress medicine is stopped, you will feel back to normal very quickly.
Are there any risks in having the exercise echo?
A Stress Echo scan is extremely safe, but there are some risks you need to be aware of. Rarely (around 1 in 1000 patients), the stress medicine may make the heart develop an abnormal rhythm. If this occurs, it will often settle down by simply stopping the stress medicine, but occasionally you may need additional treatment for this.
There is a very small risk (less than 1 in 2000) of a bad angina attack or heart attack occurring during the test.
There is an extremely small risk (less than 1 in 10,000) of developing an allergic reaction to one of the medicines used. If you have had allergic reactions to any medicine before please inform your Doctor before starting the test.
What is it?
An echocardiogram or ‘echo’ is a scan that uses ultrasound (sound waves) to produce pictures of the heart. The test is painless and without side effects. It does not use radioactivity.
Why is it being done?
An echocardiogram gives your Doctor information about how well the heart pumps and whether your heart valves are working properly. It is not able to tell your Doctor whether you have angina.
What does it involve?
You will be taken into a darkened room. The person performing the test is called a Sonographer, who may be male or female. The Sonographer will usually NOT be a doctor. This means that some questions you may have about the result may have to wait until you see your doctor in clinic.
You will be asked to undress to the waist and put on a gown that should be left open to the front. You will be asked to lie on a couch on your left hand side. If you require a chaperone, you may bring a friend or relative. Alternatively, the hospital may provide a chaperone at your request.
Stickers will be attached to your chest and connected to the machine. These will be used to monitor your heart rate during the test.
An ultrasound probe covered by a small amount of gel is placed gently on the centre of your chest and will be moved to different positions – beneath the left breast, beneath the rib cage and to the base of your neck. This provides images of your heart from a number of different angles which are then recorded.
During the echocardiogram you will hear sounds coming from the machine, which represent blood flow through the heart.
The echocardiogram will take approximately 30-40 minutes to complete.
Are there any special precautions that I need to take before the echocardiogram?
No. You can take all your medication as normal. You can eat and drink as normal.
At the end of your echocardiogram
Once the echocardiogram is complete you can get dressed and leave. There are no limitations to what you can do after the scan, for example, you may drive.
What is it?
A transoesophageal echocardiogram (TOE) is a heart scan that uses ultrasound (sound waves) to produce images of the heart. The test is painless and does not use radioactivity. It involves swallowing a soft flexible tube as the pictures are taken via the gullet.
Why is it being done?
A TOE allows your Doctor to take extremely detailed images of your heart. A TOE is often used to look carefully at the valves and the structure of the heart. The TOE will help the Doctor decide on the best treatment for your heart.
What does it involve?
This procedure is performed as a day-case.
Three people will usually be present to perform the scan: a Doctor, a Sonographer and an assistant.
You will have stickers attached, so that your heart rate can be monitored throughout the scan. You will also have your blood pressure checked, and be given oxygen. You will be able to breathe completely normally throughout the test.
You will have some local anaesthetic sprayed on the back of your throat and then asked to lay on your left hand side. A drip will be placed in your arm. If you have dentures, you will be asked to remove them before the test. Often, you will then be given some sedation to relax you, although you will not be completely asleep.
You will then be asked to swallow the TOE probe. This part may cause discomfort, but is not painful. Recorded images of the heart will then be obtained. The test will take about 20 minutes.
At the end of the procedure, the tube will be removed, your blood pressure will be checked again, and you will allowed a short period of recovery.
Are there any special precautions that I need to take before the echocardiogram?
You must NOT eat or drink anything for 6 hours before the test.
Normal medications should be taken on the morning of the TOE with a small sip of water. Please bring a copy of your prescription with you. If you are diabetic, please inform the nurses as soon as you arrive at the Day Care unit. If you are on Warfarin, your INR should have been checked within the preceding 24 hours (we will arrange on the day if needed).
Please inform your Doctor if you have any problems with swallowing, or if you have had any bleeding from your stomach. This may prevent the TOE from being performed.
At the end of your echocardiogram
After the TOE, you will be monitored for a short period of recovery. When you are fully alert and the sensation has returned to your throat, you will be allowed a drink.
You will be allowed home when you are fully awake, usually 2-3 hours after the procedure. Before you are discharged, the results of the scan will be explained to you.
If you have been given sedation, you should NOT drive or operate heavy machinery for the remainder of the day. You should be accompanied home by a friend or relative. You can go back to normal activities the following day.
Are there any risks in having the TOE?
The TOE scan is extremely safe, but there are some risks you need to be aware of.
It is not uncommon to have a sore throat after the procedure. This may last for a day or two.
Occasionally the throat may bruise or bleed slightly.
There is a small chance of inhaling stomach contents during the procedure. This is why it is important that you do NOT eat or drink anything for six hours before the procedure.
There is an extremely small risk (less than 1 in 10,000) of damaging or tearing the gullet. In extreme circumstances this may require an operation to repair the damage.
Your Doctor would not be requesting the TOE unless he or she felt it would help in deciding on the best treatment for your heart. If you have any questions regarding the TOE please contact your Doctor’s secretary, or this unit.
Discussion with Dr McAloon is important to answer any questions that you may have. For information about any additional symptoms you may be suffering from that are not featured within the site, please contact us for more information.